Brains! Neuroinflammation in ME/CFS
ME/CFS classified as neurological disease by World Health Organization (WHO). Here's why.
Myalgic Encephalomyelitis. It’s right there in the name: inflammation of the brain and spinal cord. ME is a neurological disease impacting the central nervous system. Yet, you’d never know it based on how we’re often treated by doctors. I want to focus on this part of the disease because it feels minimized, misunderstood and poorly managed in treatment protocols. My own experience has shown me the power of incorporating neurological treatments for moving the needle.
Thankfully, there’s been some amazing research into this field over the past ten or so years. We also have a growing community that is increasingly connected. We’ve learned anecdotally from our own experiences how much neurological interventions can help. Personally, I feel a tremendous difference since treating the neurological symptoms.
The information below is a tiny window into the research that’s taken place. This is meant to provide a general overview of what has been hypothesized, tested and confirmed. My summaries and interpretations may be imperfect at times, as I’m not a neuroscientist. I encourage you to check out these papers and researchers yourself, if you are able.
So, what’s going on with our brains and nervous systems? I would argue Jarred Younger is the first stop for anyone interested in answering this question. Dr. Younger is the director of the Neuro-inflammation, Pain and Fatigue Laboratory and is also a member of the UAB PAIN Collective. He also happens to be an extraordinarily gifted science communicator.
The first video I posted below is a bit dated, but I find it to be an incredibly accessible 20-minute tour of neuroinflammation. Dr. Younger first explains what’s happening in the brain when neuroinflammation occurs and how this process can make a person feel sick. The “priming” of certain immune cells in the brain can cause those cells to transition into an activated state, causing inflammation. This process can happen quickly and in response to lots and lots of things—making one feel as if they “get sick” repeatedly, even throughout a single day. Sound familiar?
He then goes on to discuss some of his research findings in people with ME/CFS (again, this video is dated, and he now has much more research). A few of the take-aways:
Lactate, a direct indication of inflammation in the brain, was found to be elevated in multiple regions of the brain that correspond to ME-specific symptoms.
Lactate was found to be about 4x greater than normal in ME patients, compared to healthy controls.
Brain temperature, another direct indication of inflammation, was found to be significantly elevated in the ME patients. This suggests the metabolic activity in the brain is greater than the blood’s ability to cool the brain—that’s neuroinflammation.
On average, the ME brain was one-degree Fahrenheit warmer than the control, which is significant for the brain. And the same regions with elevated lactate are showing up with elevated temperature!
In this video, Jarred refers to the very first study from 2014 that documented neuroinflammation in the brains of ME patients, that study is here if you’d like to take a look. A really important note is that Jarred’s brain scans corroborated that 2014 study by finding the same regions of the brain impacted.
Watch for yourself!
If you’re interested in Jarred’s research, he has a very accessible YouTube video series here.
2023 Meta-Analysis
Fast forward to 2023 to a meta-analysis that was conducted on neuroinflammation in ME/CFS. A meta-analysis is a statistically robust evaluation of multiple studies focusing on a single topic. It basically “studies the studies” in order to pull together statistically significant findings that cross study groups and methods. You can find the analysis here:
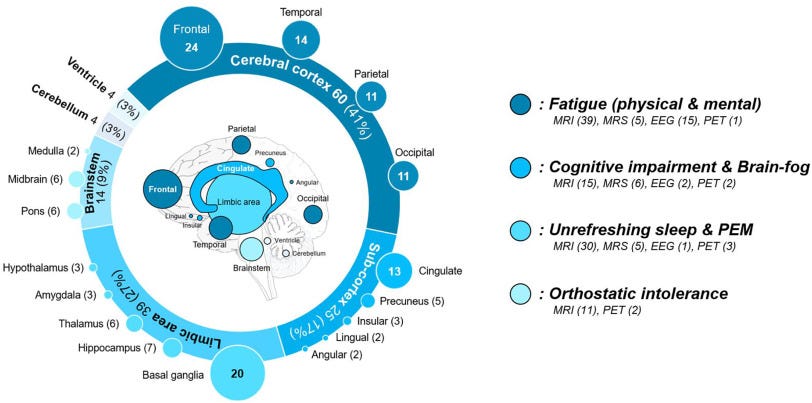
In this meta-analysis, 131 studies were considered, and 65 studies were ultimately selected based on inclusion criteria. From those 65 studies, 3,244 people participated—some with ME/CFS and some as healthy controls. Some of the findings include:
Among the observed brain areas, the cerebral cortex exhibited the highest frequency, accounting for 41% of the total observations. This was followed by the limbic area at 27%, sub-cortex at 17%, brainstem at 9%, and cerebellum and ventricles, both at 3%.
Here’s how that breaks down by common symptoms:
A significant reduction in global brain activity among patients diagnosed with ME/CFS when compared to control subjects. This was measured by an in-depth analysis of MRI data, encompassing parameters such as blood flow, blood oxygen level–dependent signals, functional connectivity, and regional volume.
Upon conducting an analysis of MRS-derived brain metabolites, serving as indicators of neuroinflammation, notable findings emerged among ME/CFS patients. Specifically, ME/CFS patients exhibited significant elevations in lactate concentration and the choline/creatine ratio demonstrated a marked increase in ME/CFS patients.
In the context of an EEG-based meta-analysis, significant findings emerged regarding total brain waves among ME/CFS patients. Specifically, ME/CFS patients exhibited significant decreases in total brain waves as evidenced by data pooled from 17 studies encompassing 765 participants, when compared to control subjects.
An examination of two PET studies employing TSPO radioligands, which serve as biomarkers of microglial activity, revealed divergent patterns in all six examined brain regions, which included the cingulate cortex, hippocampus, amygdala, thalamus, midbrain, and pons.
Finding these kinds of collaborative data sets is critical to establishing a body of scientific work. It promotes more research, becomes an area of greater interest and, hopefully, translates to clinical understanding!
What Happens in Vagus
Right up there with Dr. Younger, in my opinion, is Michael VanElzakker for his studies into the brain and nervous system. Dr. VanElzakker is a neuroscientist affiliated at Massachusetts General Hospital, Harvard Medical School, and Tufts University. He conducts his imaging research at the Martinos Center for Biomedical imaging.
In the 30-minute video below, Dr. VanElzakker covers a couple key topics that help explain the brain-body connection. He emphasizes the vagus nerve in its role communicating between the body and the brain and how this likely impacts people with ME. Through scanning technology, we can observe the impact on the brain from the vagus nerve signaling problems from the body. The vagus nerve communicates “sickness” in the body up to the brain and this may be one cause of neuroinflammation.
Interestingly, one of the regions Dr. VanElzakker points out was recently discussed in a study titled “A body–brain circuit that regulates body inflammatory responses.”
The study was discussed by Dr. Younger in the video below, where he also shares his thoughts on how studies like this can be used to advance our understanding of ME.
Yet another study has examined the brain-body connection with some very interesting findings nicely summarized in a recent Health Rising post, How Neuroinflammation May Be Knocking out the Muscles in Long COVID, ME/CFS and Fibromyalgia.
In this study, the authors introduced a variety of triggers (bacterial infections, the SARS-CoV-2 protein ORF3a, and the neurotoxic protein Aβ42 found in Alzheimer’s) to produce neuroinflammation in the brains of fruit fly and mice. While the study was done in fruit flies and mice, this pathway appears to be highly evolutionarily conserved, i.e. this core pathway is present in many species.
Each animal responded to the introduction of these substances with a clear increase in muscle fatigue and reduced endurance. Introducing these stressors into the brain triggered increased levels of reactive oxygen species (ROS), or free radicals which then triggered the production of the IL-6 cytokine, which then found its way to the muscles, where it turned on genes that turned down energy production.
For the first time, inflammation in the brain was shown to reduce muscle mitochondrial activity and endurance dramatically. No exercise was needed to shut down the muscles. All it took was neuroinflammation.
Professor Warren Tate, a Professor of Biochemistry at the University of Otago, New Zealand, also published a comprehensive paper titled Molecular Mechanisms of Neuroinflammation in ME/CFS and Long COVID to Sustain Disease and Promote Relapses.
“We propose the hypothesis that following the initial stressor event, the subsequent systemic pathology moves to the brain via neurovascular pathways or through a dysfunctional blood-brain barrier (BBB), resulting in chronic neuroinflammation and leading to a sustained illness with chronic relapse recovery cycles. Signaling through recognized pathways from the brain back to body physiology is likely part of the process by which the illness cycle in the peripheral system is sustained and why healing does not occur.”
“In Your Head”
Any neurologist who treats MS should absolutely treat ME. The massive gap in medical care from neurologists is confounding given the clear involvement of the brain. I know, add it to the list of specialists we should be able to tap for care! Personally, I believe neurological interventions may have the power to provide the most therapeutic benefits for some (many?) of us (probably in combination with other things).
In a previous post, I discussed my own treatment plan and definitely feel that’s been the case for me. You can revisit that here. The treatments I would point to include low dose naltrexone, low dose abilify, guanfacine, dextromethorphan, vagus nerve stimulation. As we all know, we’re an incredibly diverse group and each of us has to find the right treatment combination that works individually. I hope, though, if you’re discussing symptoms and treatments with your doctor, the resources and information in this post might provide some context and direction.
I’ll also point you to my previous post about applying for disability because I discuss the value of highlighting the neurological side of ME. If you’re considering disability, I encourage you to check out my discussion on getting a neuropsychological test, which I paired with a qEEG.
Next time someone expresses doubt or cynicism about ME, you can set them straight with some brain science! Take care, as always.


Thanks for this awesome post full of relevant resources! This should be an ME primer for everyone.
Thank you so much for this valuable information to help us understand whats happening in our bodies, and to help us communicate most effectively with doctors.